II. How to Use
When to Use
Patients ≥21 years old presenting in the emergency department with acute chest pain concerning for ACS.
Pearls / Pitfalls
-
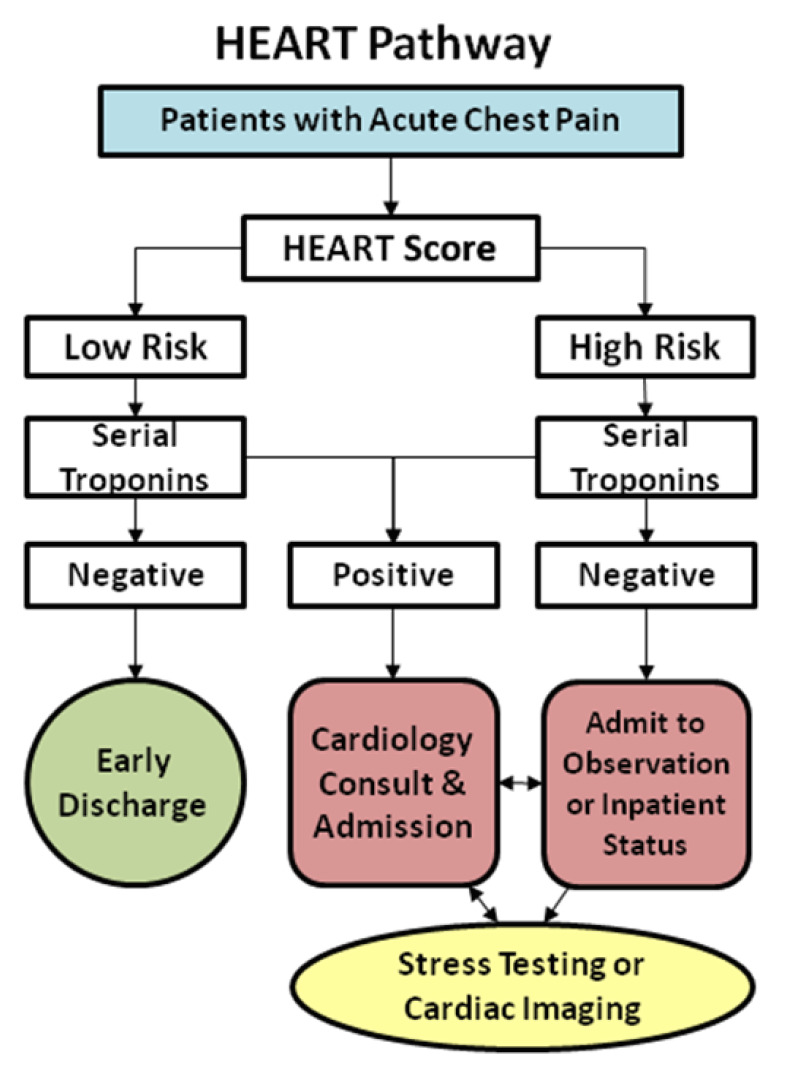
The HEART Pathway was designed to aid in efficiently evaluating patients with acute chest pain using the previously validated HEART Score. The HEART Pathway builds on the HEART Score by including a 3-hour troponin into an accelerated diagnostic pathway (ADP).
-
Interobserver variability of the HEART Score is a known issue, and the HEART Pathway adds specificity and slight modifications to the scoring rubric.
-
Identifies patients who are safe for early discharge as low risk for acute coronary syndrome versus those who need observation, admission, and/or potentially emergent cardiology assessment.
-
While patients with new ischemic changes on EKG may be classified as low risk using the HEART Pathway, the creators did not consider those patients low risk in their validation study. New ischemic EKG changes require further workup and should not be deemed low risk.
-
Similarly, in their validation study, the creators of the HEART Pathway did not rely on this clinical decision tool in patients with known coronary artery disease as their disease state puts them at significantly increased risk of ACS.
-
Designed for patients presenting to the emergency department with chest pain, this ADP has not been tested in already-hospitalized patients with chest pain.
Why to Use
-
Chest pain is one of the most common and potentially life-threatening chief complaints in emergency medicine. Many patients presenting with chest pain undergo unnecessarily extensive and costly evaluations to rule out ACS. The HEART Pathway can reduce the number of prolonged stays and invasive testing, while maintaining high sensitivity and negative predictive value for ACS.
-
Unlike other scoring systems such as TIMI or GRACE, the HEART Pathway is designed to predict the likelihood of ACS in the patient presenting to the emergency department with acute chest pain. TIMI and GRACE are used to risk stratify patients who have been already diagnosed with ACS.
III. Next Steps
Advice
-
The HEART Pathway is an ADP. It is not designed to replace clinical judgment.
-
Any patient with a concerning presentation or clinical progression should receive workup and treatment based on the clinician’s discretion, regardless of the HEART Pathway’s predicted risk.
-
Shared decision making is a crucial part of further management after ACS risk has been determined, especially in patients with moderate risk who are recommended for observation and comprehensive cardiac evaluation. There is notable risk involved with hospitalization as well as risk of false-positive or non-diagnostic testing that would result in invasive procedures such as cardiac catheterization. The patient should be presented with the risk of both missed ACS and hospitalization for further workup. See the Chest Pain Choice Decision Aid from Mayo Clinic for risk-specific decision aids.
-
Any patient presenting with chest pain and subsequently discharged should be informed that even with a negative workup, there is still a small risk of ACS. However, with a <1% risk of ACS within 30 days, it is important to emphasize that automatic outpatient cardiac risk stratification carries a higher risk of false-positive than a true positive, and could result in unnecessary invasive procedures (such as cardiac catheterization) that carry inherent risks. Instead, patients should be set up with close primary care follow-up and given extensive return precautions prior to discharge.
Management
-
Low risk patients with a follow-up troponin at 3 hours after ED presentation can be considered for safe discharge home with appropriate follow-up.
-
High risk patients require admission, observation, serial cardiac biomarkers and EKG, and/or cardiology consult.
Critical Actions
-
Clinician judgment should prevail, even if patients are deemed low risk by the HEART Pathway. If there is some other cause for concern of acute cardiac syndrome, workup should be individualized to the patient.
-
All patients presenting to the ED with chest pain concerning for ACS should receive aspirin unless there is an absolute contraindication (known allergy, active bleeding, or the patient has received a therapeutic dose prior to arrival).
IV. Evidence
Evidence Appraisal
The HEART Pathway was developed by Mahler et al in 2015 in a randomized controlled single-center trial.
-
Control arm was managed at the discretion of care providers encouraged to follow American College of Cardiology/American Heart Association guidelines for acute chest pain.
-
The use of the HEART Pathway in this study was designed to mimic the real world in that it was used as an ADP. Patient care was at the discretion of the health care provider and not mandated by the outcome of the HEART Pathway.
-
n = 282, with 141 patients in each treatment group.
-
Primary outcome: rate of objective cardiac testing (stress test, coronary CTA, or invasive coronary angiography) within 30 days of presentation.
-
Secondary outcomes: early discharge rate, index length of stay, cardiac related recurrent ED visits, and nonindex hospitalization at 30 days.
-
The rate of objective cardiac testing in the HEART Pathway group was 12% less than the usual care group.
-
The rate of early discharge in the HEART Pathway was 21% higher than the usual care group.
-
The index length of stay was 12 hours shorter using the HEART Pathway.
-
There was no significant difference between the two groups for cardiac related recurrent ED visits or nonindex hospitalization at 30 days.
-
No patients identified for early discharge in either group had missed MACE during the first 30 day follow up period.
-
Study was not powered to adequately detect difference in major adverse cardiac event (MACE) between the two study groups.
Mahler and colleagues (2017) also published a secondary analysis looking at high sensitivity cardiac troponin (hs-cTnI and hs-cTnT).
-
Compared risk stratification using cardiac troponin I (cTnI) vs. high sensitivity cardiac troponin (hs-cTnI and hs-cTnT) in calculating the HEART Pathway score.
-
n = 133, patients had blood samples sent for cTnI, hs-cTnI, and hs-cTnT.
-
All of the troponin assays had poor sensitivity for predicting MACE when used separately from the HEART Score.
-
There was no difference in the predicted risk of MACE between the use of serial cTnI and 3-hour hs-cTnI in the HEART Pathway.
-
Using hs-cTnT in the HEART Pathway led to one patient with an NSTEMI to be misclassified as low risk.
-
The study found the HEART Pathway using serial cTnI or 3-hour hs-cTnI to have sensitivity and NPV of 100% for 30-day MACE.
-
Although hs-cTnT use in the HEART Pathway caused an NSTEMI to be misclassified as low risk, the reduction in sensitivity was not statistically significant, given the small study population. The authors recommend further appropriately-powered studies to determine small differences in the accuracy of the high sensitivity troponin assays.
-
High risk features of chest pain: Retrosternal pain, pressure, radiation to jaw/left shoulder/arms, duration 5–15 min, initiated by exercise/cold/emotion, perspiration, nausea/vomiting, reaction on nitrates within mins, patient recognizes symptoms. Low risk features: well localized, sharp, non-exertional, no diaphoresis, no nausea or vomiting, and reproducible with palpation.
-
Repolarization abnormalities, non-specific T wave changes, non-specific ST-segment depression or elevation, bundle branch blocks, pacemaker rhythms, LVH, early repolarization, or digoxin effect.
-
lschemic ST-segment depression or new ischemic T-wave inversions.
-
HTN, hypercholesterolemia, DM, obesity (BMI >30 kg/m2), smoking (current, or smoking cessation ≤3 mo), positive family history (parent or sibling with CVD before age 55).
-
Use local assays and corresponding cutoffs.